Israel is currently leading the way with COVID-19 vaccination; 62.5% of people have had at least one dose of vaccine. The UK isn’t far behind, with 1 in 2 people having had a COVID-19 jab. Given the UK is only vaccinating adults, it’s actually vaccinated 2 in 3 people. That’s a substantial proportion of the population, with all vulnerable adults having been offered a jab. 💉
Thanks to a lockdown and vaccinations, positive coronavirus tests and related deaths have been falling since January in Israel. The UK has a population of 68 million people, much larger than Israel’s 9 million, so how are things working out here?
Has the UK beaten coronavirus?
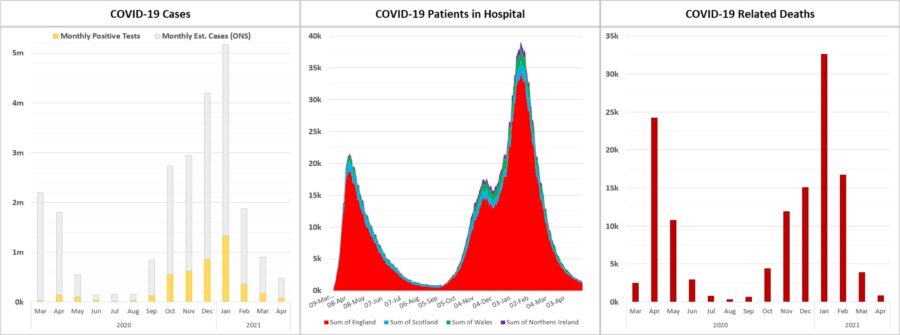
The UK went into a lockdown at the start of January. Schools re-opened in March, with restrictions gradually easing since then. Around the same time, testing capacity was dramatically increased, improving detection of asymptomatic cases. On one day in March nearly 2 million coronavirus tests were conducted! Despite this, the number of positive tests still continues to fall, as does the number of people in hospital with coronavirus and COVID-19 related deaths.
So how does this relate the the vaccine roll-out, what were the key milestones?
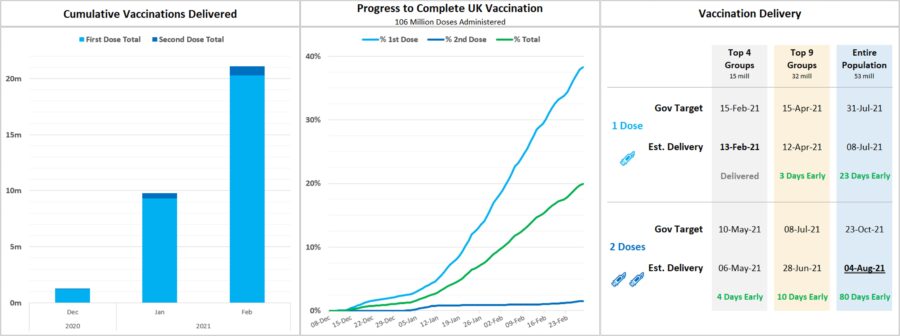
The UK split its 53 million adult population into three categories:
- Priority cohorts 1 to 4 – 15 million people
- This group included over 70s, the Clinically Extremely Vulnerable (those shielding), as well care home residents, and those who work in care homes, health care and social care
- Priority cohorts 5 to 9 – 17 million people
- This group included over 50s, as well as anyone deemed to be at risk due to their job or social circumstances
- General population – 21 million people
- Everyone else
Cohorts 1 to 4 account for around 88% of all COVID-19 deaths, while groups 1 to 9 account for 99% of all deaths. So once 32 million people have been offered a jab, there will be a significant reduction, near elimination, in the likelihood of deaths from COVID-19.
That’s huge!
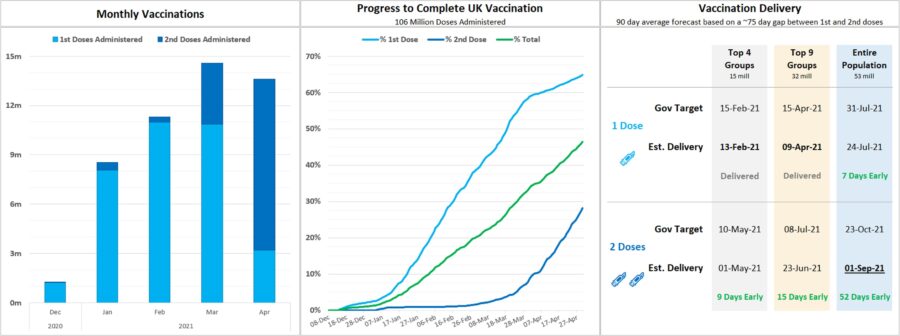
So where are we at? Currently, around 35 million people have had a first jab, 16 million of which have also had a second. That’s a mix of the AstraZeneca, Pfizer, and Moderna vaccines.
That means all the most vulnerable groups (accounting for 88% of deaths) are fully vaccinated – bar those who’ve refused a vaccine.
Here are some charts showing the UK’s progress. The delivery forecast is based on the 90-day average of vaccinations administered.
The data is all going in the right direction, and I feel quite confident in saying: yes, COVID-19 vaccines do work and the UK is beating coronavirus. Vaccinations are effective at reducing hospitalisation, death, but also at reducing virus transmission.
Points to consider
The more people who catch COVID-19 (globally) the greater the risk of new variants or strains, these could potentially be more harmful, transmissible and vaccine-resistant, but they could also be more benign. Until we’ve stamped out COVID-19 globally, there will be a risk that even a highly vaccinated country could go backwards.
There are also ethical questions around vaccine supply. The UK provided funding and support to multiple vaccine programmes very early on, helping it to secure supplies of several vaccines. Now it’s vaccinated it’s most vulnerable, is there a case for it to gift or sell on doses to other countries with fewer supplies and higher need? Countries like India, which is struggling with the pandemic at the moment. A vaccine given to a not-at-risk adult may stop 1 death in 100,000 in the UK, whereas if given to someone at risk in India right now, it could save 1 in 1,000. It could also free up health care capacity, to support others who haven’t been vaccinated yet.
Wherever you are in the world, there is cause for optimism.
Vaccines work and we are turning the tide on COVID-19! 😊